

Affiliations
ABSTRACT
Radicular cysts are the prevailing inflammatory jaw cysts. Historical surgical modalities, including marsupialization and enucleation, have been conventionally employed to optimise postoperative conditions and expedite the healing trajectory in the affected regions. The fundamental surgical objective is the eradication of periapical disease, instigation of bone regeneration, and facilitation of periapical tissue convalescence.
Autologous platelet-rich fibrin (PRF) has emerged as a promising regenerative biomaterial with profound potential for expediting healing in oral surgical defects. PRF, a third-generation platelet concentrate, autogenously derived from patient’s own blood, exhibits notable utility in root coverage applications. This case series aims to elucidate the impact of PRF on the resolution of bone defects following radicular cyst enucleation. A three-month follow-up manifested a discernible enhancement in bone density, thereby affirming the substantive efficacy of PRF in the treatment of bone defects.
Key Words: Periapical disease, Radicular cysts, Enucleation, Platelet-rich fibrin.
INTRODUCTION
The most common inflammatory cysts in the maxillofacial region are radicular cysts, which originate from the epithelial remnants of Malassez (ERM) of the periapical ligament. These cysts initiate through a proliferative response induced by inflammation, which is a consequence of the pulpal decay of a non-vital tooth. This process ultimately leads to the formation of a periapical granuloma.1
The pathogenesis of cystic transformation commences with the onset of inflammation and progresses through subsequent cystic expansion, thereby affecting adjacent osseous structures and surrounding anatomical entities. Toxins emanating from the necrotic pulp accumulate at the apical foramen, inciting localised periapical inflammation.2
The management of radicular cysts is contingent upon factors such as size, location, dimensions, and proximity to vital structures, with therapeutic modalities encompassing both nonsurgical and surgical interventions, including marsupialization and enucleation.1 Notably, radicular cysts have been associated with the induction of consequential bone defects.
Platelet-rich fibrin (PRF) is a blood-derived biomaterial rich in platelets and growth factors such as platelet derived growth factor (PDGF), transforming growth factor-beta (TGF-β), insulin-like growth factor (IGF), epithelial growth factor (EGF), fibroblastic growth factor (FGF), and bone morphometric protein (BMP). These components play vital roles in cell growth, differentiation, and tissue formation. With a molecular structure conducive to cell migration and low thrombin concentration, PRF is optimal for promoting endothelial cell and fibroblast migration. This makes it suitable for applications requiring enhanced tissue healing, regeneration, and remodelling.
PRF benefits include facilitating haemostasis, promoting angiogenesis, supporting osteoblastic proliferation and differentiation, providing postoperative protection, expediting tissue integration, maturation, and remodelling, and enhancing bone density. Overall, PRF stands out as a promising biomaterial for medical and dental applications, particularly in tissue healing, regeneration, and bone grafting. The authors shared their experience in the practical application of PRF, specifically in the surgical management of large radicular cysts, highlighting its potential as an effective biomaterial in various medical and dental contexts.Top of Form
CASE 1:
A 48-year female patient presented to the endodontics department with a complaint of a draining sinus from the maxillary left lateral incisor and Grade II mobility. A periapical radiograph revealed a well-defined radiolucency. Electric pulp test confirmed non-vital upper left central incisor and lateral incisor. Subsequently, root canal treatment (RCT) was performed on the left central and lateral incisors. However, at the six-month follow-up, the patient continued to experience persistent pus drainage from the stoma associated with the maxillary left lateral incisor (Figure 1, A and B). Grade II mobility and excessive bone loss were associated with lateral incisors.
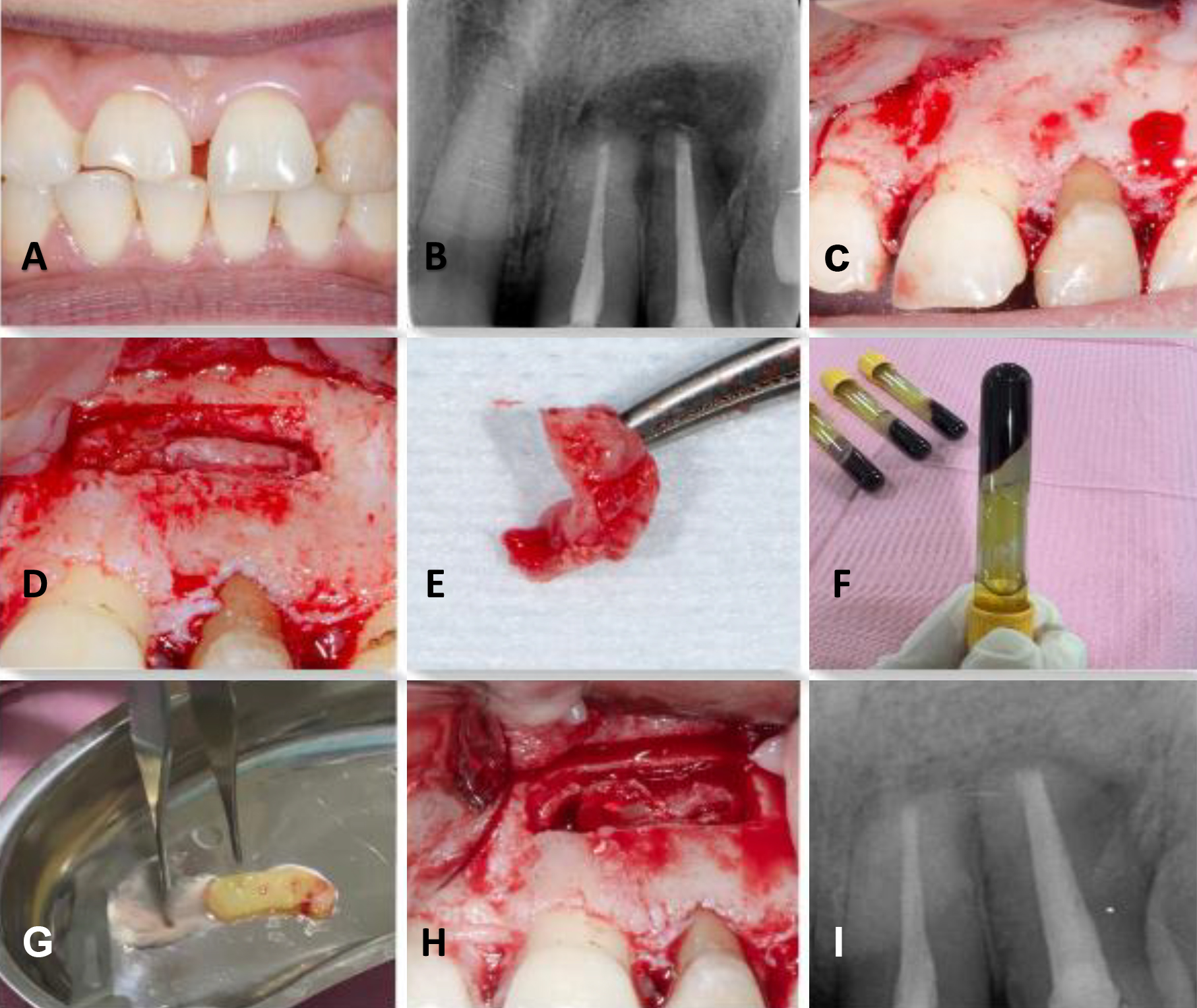 Figure 1: (A) Intraoral view (B) Preoperative radiograph (C) Flap Elevation (D) Bony window creation (E) Enucleation Process (F,G) Formation of platelet-rich fibrin (PRF) (H) PRF placement (I) Three months postoperative periapical radiograph.
Figure 1: (A) Intraoral view (B) Preoperative radiograph (C) Flap Elevation (D) Bony window creation (E) Enucleation Process (F,G) Formation of platelet-rich fibrin (PRF) (H) PRF placement (I) Three months postoperative periapical radiograph.
A comprehensive treatment plan was devised, involving the enucleation of the cyst and the placement of PRF in the bony defect. Additionally, an apicectomy, involving the resection of the apical end by 3 mm, was planned. Ultrasonic tips were employed for the procedure, along with retrograde preparation and the placement of Mineral Trioxide Aggregate (MTA) filling. Following the enucleation, histopathological analysis revealed the presence of a radicular cyst (Figure 1, C-E).
To prepare platelet-rich fibrin PRF, 5 ml of whole venous blood was collected in each of two sterile vacutainer tubes without anticoagulant. The tubes were centrifuged at 3000 rpm for 10 minutes, resulting in three layers: the lower red fraction (red blood cells), the upper straw-colored layer (cellular plasma), and the middle fraction, which was collected 2 mm below the lower dividing line, representing the PRF (Figure 1, F and G). The collected PRF was then packed in the bony defect to promote local wound healing (Figure 1H). The wound was closed with 4/0 polyglactin sutures.
At three-month follow-up, the patient showed excellent radiographic and clinical outcomes having no signs of infection and mobility of teeth (Figure 1I).
CASE 2:
A 35-year female patient with no notable medical history presented with a complaint of pain in the right side of the lower jaw. The patient reported a history of trauma to the same side of the jaw about 10 years ago. Intraoral examination revealed a broken-down root of the lower right canine with no mobility and swelling in the canine area. On sensibility testing, lateral incisor and first premolar were vital and non-mobile. Periapical radiograph exposed a pear-shaped, well-corticated periapical radiolucency extending around the roots of the lower right lateral incisor, canine, and first premolar region (Figure 2, A and B).
Further evaluation using cone-beam computed tomography (CBCT) identified a round-shaped lytic lesion with regular margins in the anterior region of the mandible. The dimensions of this lesion were 2 × 2 × 0.5 cm (bucco-lingual × mesiodistal × corono-apical), causing notable expansion in the buccal bone. The treatment plan included extraction of broken-down root no. 43, enucleation of the cyst, followed by concurrent placement of PRF. The wound was closed primarily with 3/0 polyglactin sutures. Histopathological analysis of the specimen confirmed the diagnosis of a radicular cyst. On three months follow-up, full bony refill of the defect was appreciable on the periapical radiograph (Figure 2, C and D).
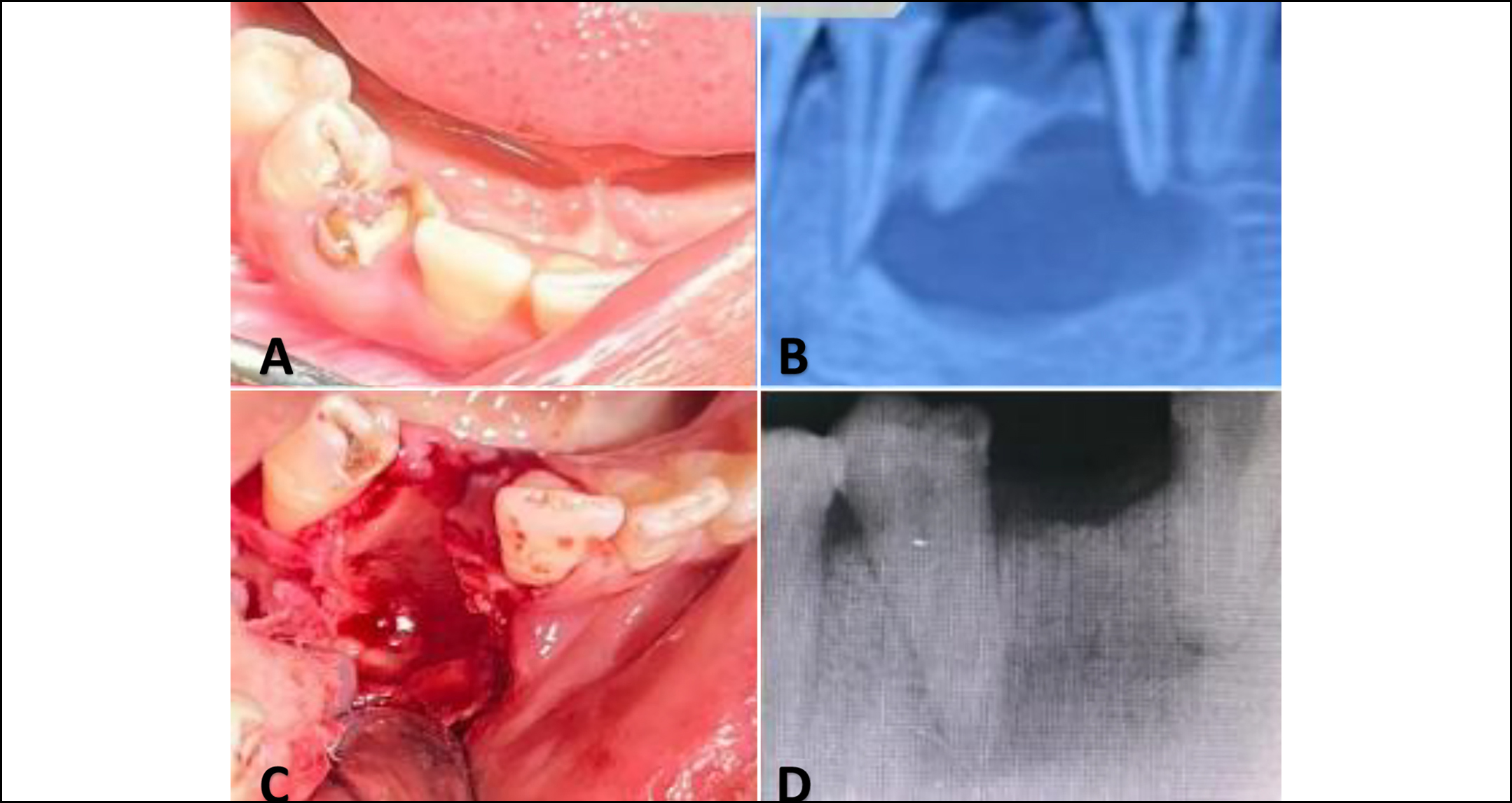 Figure 2: (A) Intraoral view (B) Preoperative radiograph (C) Cyst enucleation and canine root removal (D) Three-month postoperative radiograph.
Figure 2: (A) Intraoral view (B) Preoperative radiograph (C) Cyst enucleation and canine root removal (D) Three-month postoperative radiograph.
DISCUSSION
The preparation procedure for PRF is straightforward, and the equipment needed is the same as that used for PRP. 2
Radicular cystic lesions progress asymptomatically, marked by crepitations, subsequent erosion, and the development of fluctuations in the overlying soft tissue. The adjacent bone undergoes thinning, acquiring a springy feel and eggshell-like crackling, resulting in the expansion of the cortical plate. Palpation of the alveolar process reveals a paper-like texture.3
PRF, resembling a fibrin meshwork, plays a vital role in facilitating cell movement and proliferation. Derived from anticoagulant-free blood, PRF generates various growth factors, including PDGF and TGF-β. Widely employed in oral and maxillofacial surgery, periodontal surgery, ear-nose-throat surgery, and plastic surgery, PRF serves as a surgical adjuvant, particularly noted for its role in promoting the healing of surgical wounds with substantial bony defects resulting from radicular cysts.4
Choukroun et al. introduced PRF in France, representing a newer class of platelet concentrate.5 Its simplified processing technique, which does not involve complex blood handling, positions it superior to platelet-rich plasma (PRP). PRF finds application in promoting wound healing, bone growth, graft stabilsation, wound sealing, and hemostasis. The well-organised fibrin matrix enhances its ability to efficiently guide stem cell migration and the healing process. Recent in vitro studies examining the release of growth factors from PRF, along with in vivo results, suggest an opportunity to optimize its clinical use. Dohan et al. noted a slower but more effective release of growth factors from PRF as compared to PRP, emphasising improved healing properties.6 Kawamura and Urist proposed that PRF may serve as a supportive matrix for BMP.7
The conventional approach to cyst management involves traditional orthograde RCT. However, for large and extensive cysts, alternative interventions such as marsupialization, decompression, and surgical enucleation may be necessary.8 The contemporary paradigm in periapical cyst management leans towards nonsurgical strategies.9 Long-term monitoring is imperative, as cyst reossification typically requires up to two years. This comprehensive approach ensures effective management and resolution of large radicular cysts while minimising associated pain and facilitating optimal healing.10
The integrated approach aimed to address both the cystic lesion and the associated endodontic issues, highlighting the importance of a multidisciplinary strategy in the management of complex cases. The utilisation of PRF and precise surgical techniques, including apicoectomy and retrograde filling, demonstrates a thorough and targeted intervention for optimal patient outcomes.
The utilisation of PRF as part of the surgical intervention demonstrates a contemporary approach aimed at enhancing the regenerative potential and promoting optimal healing outcomes.
In conclusion, the current case series verifies that the combination of PRF resulted in positive regenerative outcomes and satisfactory functional recovery. This approach may prove to be more efficient and cost-effective compared to other available regenerative materials. Therefore, it stands out as a preferred treatment option due to its economic feasibility, functional benefits, and widespread accessibility of required equipment.
ACKNOWLEDGEMENTS:
Special thanks to Dr. Muhammad Israr, Dr. Asfand Ali Khan, Dr. Sara Bano, and Adeena Sajid for their contribution.
PATIENTS CONSENTS:
Written and oral informed consents were obtained from the patients in this study.
COMPETING INTEREST:
The authors declared no conflict of interest.
AUTHORS’ CONTRIBUTION:
UR, MAA: Planning, critical review, material analysis, conception of study, study conduction interpretation, and manuscript writing.
REFERENCES